MRD Negativity Is the Deepest Response Currently Measured in Multiple Myeloma7,8
Level of Tumour Burden8,9*
 Normal cell
Normal cell Malignant cell
Malignant cell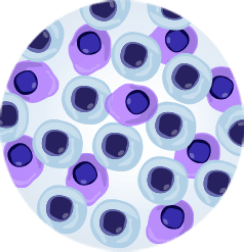
PR
(total myeloma cells: ~1 x 109)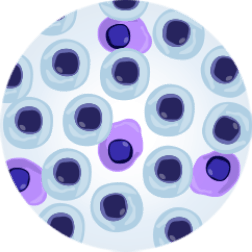
VGPR
(total myeloma cells: ~1 x 108)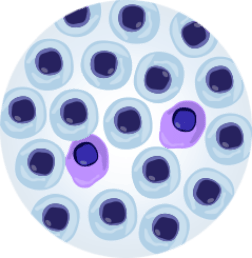
CR
(total myeloma cells: ~1 x 107)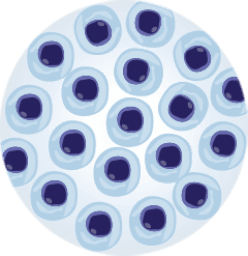
MRD-
(total myeloma cells: 0 to 106)A patient who is MRD negative has an undetectable level of malignant cells in the bone marrow at a minimum sensitivity of 10-5†
Deeper treatment responses are associated with improved outcomes3 —read more below
*While standard response categories (PR, VGPR, and CR, as noted in IMWG response criteria) are determined by measuring M-protein or free light chain levels in urine and blood samples, MRD status is determined by a direct measure of malignant cells in the bone marrow. IMWG criteria do not include tumour cell count when defining PR, VGPR, and CR.8
†Because of limitations in testing, remaining malignant cells may be undetectable at lower levels of sensitivity.3,8
MRD- is associated with improved rates of survival in NDMM and RRMM3
In a large meta-analysis evaluating patients with NDMM and RRMM, patients achieving MRD- experienced significantly longer OS and PFS vs MRD+ patients3
TRANSPLANT-ELIGIBLE NDMM: MRD- IS ASSOCIATED WITH PROLONGED OS VS MRD+
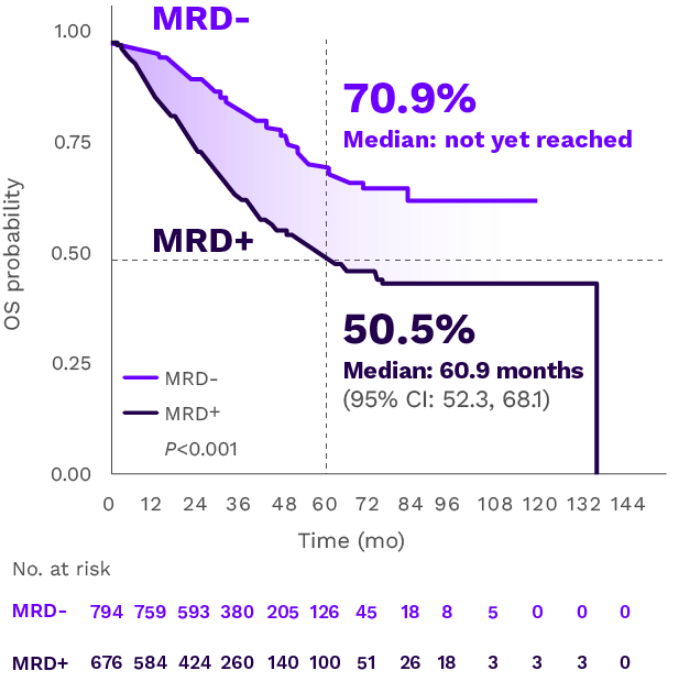
Adapted from Munshi NC et al. Blood Adv. 2020.
Five-year OS rates were 70.9% for MRD- patients vs 50.5% for MRD+ patients.3
The same trend toward improved survival was observed among patients with transplant-ineligible NDMM (N=1268) where MRD- was also associated with significantly improved OS vs MRD+ (HR=0.40; 95% CI: 0.31, 0.51; P<0.001). In the meta-analysis, a pooled Kaplan-Meier curve for OS by MRD status was not generated because it was only reported in one study.3
TRANSPLANT-ELIGIBLE NDMM: MRD- IS ASSOCIATED WITH PROLONGED PFS VS MRD+
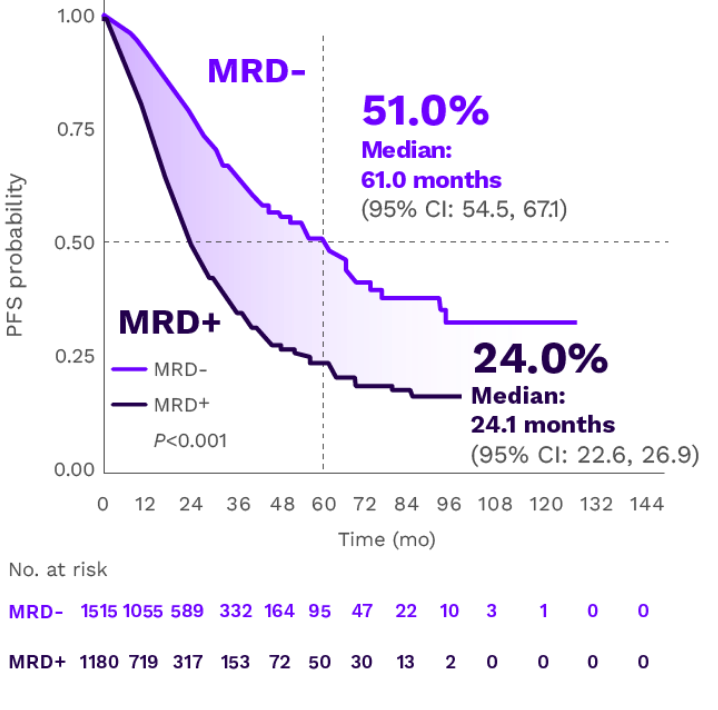
Adapted from Munshi NC et al. Blood Adv. 2020.
Five-year PFS rates were 51% for MRD- patients vs 24% for MRD+ patients.3
The same trend toward improved PFS was observed among patients with transplant-ineligible NDMM (N=2350) who achieved MRD- vs patients who were MRD+ (HR=0.32; 95% CI: 0.27, 0.39; P<0.001).3
RRMM: MRD- IS ASSOCIATED WITH PROLONGED OS VS MRD+
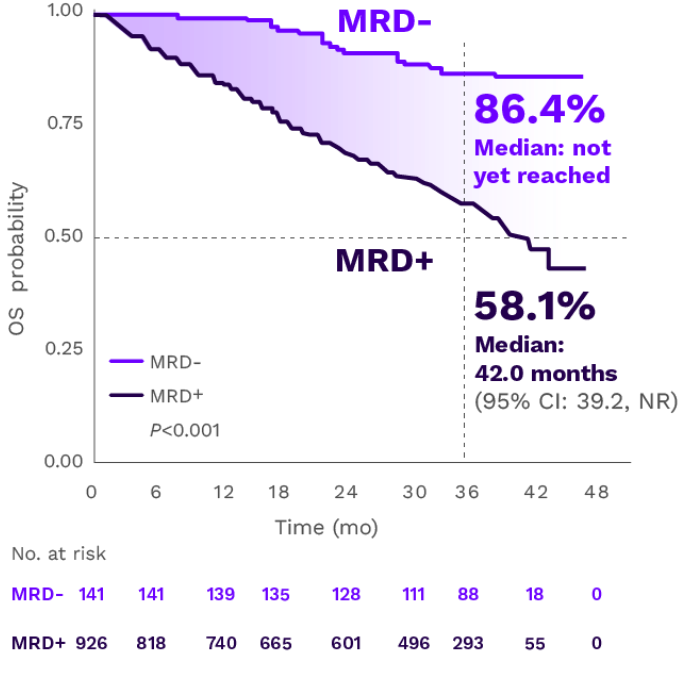
Adapted from Munshi NC et al. Blood Adv. 2020.
Three-year OS rates were 86.4% for MRD- patients vs 58.1% for MRD+ patients.3
RRMM: MRD- IS ASSOICATED WITH PROLONGED PFS VS MRD+
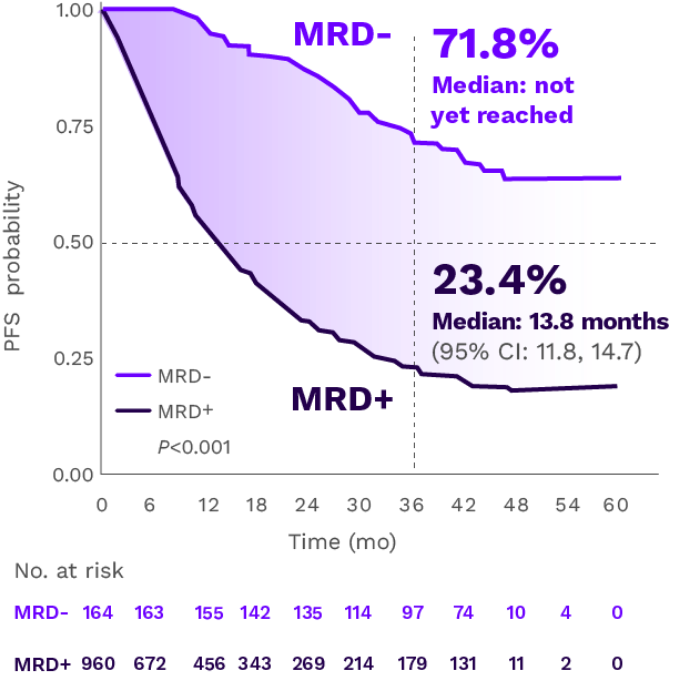
Adapted from Munshi NC et al. Blood Adv. 2020.
Three-year PFS rates were 71.8% for MRD- patients vs 23.4% for MRD+ patients.3
Achievement of MRD- may surpass CR as the strongest indicator of long-term outcomes3-5
A pooled analysis of patients with NDMM who achieved CR but remained MRD+ showed a greater risk of relapse and disease progression vs patients who achieved CR and MRD-4
Patients in CR and MRD+

MONTHS
mPFS
vs
Patients in CR and MRD-
MONTHS
mPFS
With treatment advances in MM leading to an increasing proportion of patients achieving CR, particularly in first-line therapy, the development of MRD testing has given investigators a tool to detect deeper treatment responses for a more accurate prognostic assessment.3,7
Even among patients who achieve CR, remaining MRD-positive is associated with poorer prognosis4
Hear an expert opinion and a patient’s perspective on the role of MRD- in multiple myeloma
Watch a video exploring MRD negativity as a goal of therapy of multiple myeloma
Dr Rafael Alonso discusses the relevance of MRD- as a measure of depth of response, and its importance as a treatment goal, particularly in frontline therapy. He also explores how the role of MRD- may evolve in the future, both as an endpoint and a potential tool to guide decisions in clinical practice.2
‘…we should expect that treatments delivering high rates of MRD negativity could give patients a chance for improved long-term outcomes.’
–Rafael Alonso, Complutense University, Madrid, Spain
Jim gives his perspective on MRD negativity and living with multiple myeloma
‘I realized in hearing I’m MRD negative that the treatment I’ve been having over the years is working as well as I can expect.’
–Jim, a patient with multiple myeloma who tested MRD negative in 2019
Looking to approaches that achieve high rates of MRD negativity for patients is increasingly important to ensure better outcomes1,10
Download a resource to learn moreCR=complete response; IMWG=International Myeloma Working Group; MM=multiple myeloma; M-protein=myeloma protein; mPFS=median progression-free survival; MRD=minimal residual disease; MRD-=minimal residual disease negative/negativity; MRD+=minimal residual disease positive/positivity; NDMM=newly diagnosed multiple myeloma; NR=not reached; OS=overall survival; PFS=progression-free survival; PR=partial response; RRMM=relapsed and/or refractory multiple myeloma; VGPR=very good partial response.
REFERENCES: 1. Kostopoulos IV, Ntanasis-Stathopoulos I, Gavriatopoulou M, Tsitsilonis OE, Terpos E. Minimal residual disease in multiple myeloma: current landscape and future applications with immunotherapeutic approaches. Front Oncol. 2020;10:860. 2. Dimopoulos MA, Moreau P, Terpos E, et al. Multiple myeloma: EHA-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021;32(3):309-322. 3. Munshi NC, Avet-Loiseau H, Anderson KC, et al. A large meta-analysis establishes the role of MRD negativity in long-term survival outcomes in patients with multiple myeloma. Blood Adv. 2020;4(23):5988-5999. 4. Lahuerta JJ, Paiva B, Vidriales MB, et al. Depth of response in multiple myeloma: a pooled analysis of three PETHEMA/GEM clinical trials. J Clin Oncol. 2017;35(25):2900-2910. 5. Martinez-Lopez J, Wong SW, Shah N, et al. Clinical value of measurable residual disease testing for assessing depth, duration, and direction of response in multiple myeloma. Blood Adv. 2020;4(14):3295-3301. 6. Goicoechea I, Puig N, Cedena MT, et al. Deep MRD profiling defines outcome and unveils different modes of treatment resistance in standard- and high-risk myeloma. Blood. 2021;137(1):49-60. 7. Burgos L, Puig N, Cedena MT, et al. Measurable residual disease in multiple myeloma: ready for clinical practice? J Hematol Oncol. 2020;13(1):82. 8. Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328-e346. 9. Paiva B, van Dongen JJ, Orfao A. New criteria for response assessment: role of minimal residual disease in multiple myeloma. Blood. 2015;125(20):3059-3068. 10. Landgren O, Iskander K. Modern multiple myeloma therapy: deep, sustained treatment response and good clinical outcomes. J Intern Med. 2017;281(4):365-382.