True Cost of Multiple Myeloma
True and
Complete
Cost of Multiple
Myeloma
The financial burden multiple myeloma patients face is often greater than expected when you factor in the cost of caregiving and loss of income.
Sanofi partnered with the International Myeloma Foundation (IMF) to conduct a research study to help haematologists further understand the health system and patients’ financial burdens and provide a new way to look at treatment options.
The True Cost of Multiple Myeloma (MM) report started with a systemic literature review and then discussed those findings in roundtables featuring patients, caregivers, and a variety of leaders in the MM space to gather further insights.
Read more about the four findings from the report below or download the final report.
An Economic Burden Higher Than Other Cancers
One of the biggest expenses of MM is the amount of hospital admissions, both unplanned and planned. These admissions are a significant driver behind the total cost.1
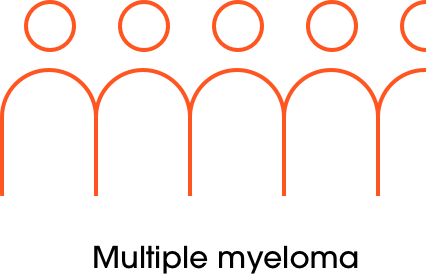
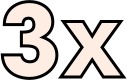
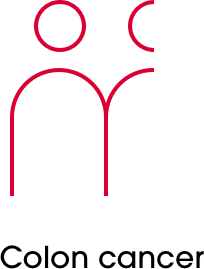
On average the number of multiple myeloma-related hospital admissions per patient is almost 3 times higher than those of colon cancer (4.5 vs 1.4, respectively).
Another consideration is the burden associated with significant productivity loss. The chart below shows the top burdens on patients and caregivers, all of which carry increased direct and indirect costs to patients and society.2
These burdens take a significant toll on patients’ productivity. A diagnosis with multiple myeloma resulted in an approximate productivity loss of €290,601 per patient over a 20-year period.3
% of patients
71%
Specialist visits
(prior 3 months)
48%
Not working due
to disease
42%
Hospital visits
(prior 6 months)
37%
Absentee days
(prior 4 weeks)
37%
Disability
compensation
34%
Family practice visits
(prior 3 months)
32%
Early retirement
19%
Working days
missed by caregiver
11%
Working now
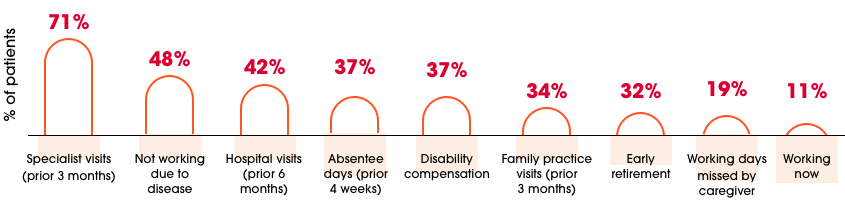
Only 11% of patients remain working post-diagnosis and treatment, with 48% of patients not working due to their disease. The research indicates that 32% of MM patients were forced into early retirement.2
More Efficacious Is More Cost-Efficient
The way healthcare costs for MM have been calculated historically does not paint the whole picture. It is time to tell a complete view because the continued progress of treatments coupled with patients being longer time on therapies, makes healthcare resource utilization and costs associated with the treatments increase, simply due to better treatments and longer time spent on therapies.
- Patients are now spending a longer time in a progression-free state because of better treatments
- The cost offsets associated with more efficacious treatments are not well documented
- A disproportionate emphasis is being placed on drug treatment costs without the consideration of potential offsetting benefits associated with treatment
In a study by Ashcroft et al. 2018, maintenance therapy was shown to delay progression to further lines of therapy and reduce resource use in a 15-month time horizon.4 For 2017:
Maintenance patients cost:
€238 - €638per month

Non-maintenance patients cost:
€438 - €1001per month
Unplanned hospital admissions represented only 10% of all MM admissions, but accounted for 55% of the total hospitalization costs.1
Optimal Treatment Pathway May Be Translated in Savings
The findings indicated that the depth and durability of tumor response to treatment can reduce overall disease cost. If the remission period is prolonged, it’s possible to achieve less active treatment and unplanned hospitalizations.5
Improved treatment outcomes may reduce the overall healthcare resource utilization and related costs.5
The evidence suggests that finding the optimal treatment pathway for patients, including selecting the optimal treatment as well as the optimal structural model, has the potential to generate cost savings for payers and patients, while improving patient experience.4
Pathway
Model
“Depending on the insurance system the patient has, it can be difficult to access more expensive treatments such as monoclonal antibodies.”
- KOL interviewee
- Medical systems vary widely by country. For many, innovative medicines are not adequately reimbursed or easily available
- The global discrepancies in access are equally important to the cost burden but are not well-described factors in publications
- New strategies are needed to improve access and outcomes for MM patients worldwide
Reducing the Cost Burden of MM
Governments, healthcare professionals, patient advocates, and industry must dedicate themselves to practical efforts that address patient cost.
Commit to researching how the variety of healthcare systems implemented globally can affect MM care and patient burden
Develop tailored solutions, not ‘one-size fits all’ programs that cannot cater to the specific needs of all MM patients
Use direct and indirect cost data to implement region-specific benefit programs to help improve access to and reimbursement of innovative treatments
Industry and governments must work together to develop frameworks that ensure available medications are efficient at reducing the economic burden on patients and society

Learn more about Sanofi’s global commitment to making a positive impact on the lives of its patients through science, research, and education.
Get more infoREFERENCES: 1. Kolovos S, et al. J Bone Oncol. 2019;17:100243. 2. Robinson D, et al. Eur J Haematol. 2017;99:119-132. 3. Jackson G, et al. Eur J Haematol. 2019;103:393-401. 4. Ashcroft J, et al. Int J Hematol Oncol. 2018;7(1):IJH05. 5. Gonzalez-McQuire S, et al. J Med Econ. 2018;21(5):450-467.